Pediatric Limb Lengthening: Corrective Surgery for Leg Length Discrepancy in Children
Children who are born with or develop differences in the length of their arms or legs can benefit from a range of treatments. These may be as simple as using adaptive footwear or as sophisticated as having limb lengthening surgery to generate new bone in the shorter limb.

Although upper extremity bones such as the humerus (the bone that connects the elbow and shoulder joints) may have length disparities, leg length discrepancy is more common.
This is especially true of the femur (thighbone), the long bone in the leg extending from the hip to the knee.
How common is leg length discrepancy in children?
Leg length discrepancy is quite common. The human body is not perfectly symmetrical, and most children have a mild leg length difference similar to the way that many people have one foot a bit longer than the other or one ear that sticks out more than the other. Overall, about 25% of people have a length difference greater than one centimeter (1cm). Only about one in a 1000 people have a difference greater than two centimeters (2cm).
What causes a child to have one leg shorter than the other?
There are numerous specific causes, but doctors separate them into two basic categories: congenital − when a baby is born with it − and acquired. Acquired limb differences are often related to an injury such as fracture, an infection such as osteomyelitis (a bacterial bone infection), an illness such as cerebral palsy or rheumatoid arthritis, or due to treatment for another condition (such as radiation therapy for cancer).
Congenital leg length discrepancy
There is a spectrum of congenital conditions that affect the femur (thighbone), which may be diagnosed at birth. These include congenital short femur and proximal femoral focal deficiency (PFFD). In other cases, the lower leg bones (the fibula and tibia) may be affected, such as in fibular hemimelia and posteromedial bowing of the tibia, respectively.
There are known genes that are associated with leg length discrepancies, but some children without these gene markers are nonetheless born with a limb difference. Congenital leg length discrepancies can sometimes occur alongside other problems, such as abnormal foot development, vascular malformations (differences in how blood vessels are formed), or other growth abnormalities.
Sometimes, a leg length difference is present from birth, but it is not obvious because both legs are small. The difference may become more apparent when the baby’s legs grow.
Predictable growth
When a baby is born with a leg length discrepancy, usually the difference between the legs stays proportional, meaning that if one leg is 10% shorter than the other, it will always be 10% shorter, even though both legs grow longer over time. The measurement difference, however, tends to get bigger over time, because 10% of a 10-cm bone (when the child is young) is just one centimeter (1cm) while 10% of a 30 cm bone (at maturity) is three centimeters (3cm).
Acquired leg length discrepancy
Problems that can result in growth arrest, limb deformities and length disparities after a child is born include:
- Infections of the bone or joint, which can occur at any time during childhood, including in the weeks immediately following birth.
- Fractures or any injury that causes damage to or leads to premature closure of the growth plate. The growth plate is the area at each end of the bone of a growing child, where new bone forms to add length.
- Exposure to radiation, which can damage the growing part of the bone (the growth plate).
- Underlying diseases and conditions whose mechanisms can affect growth. For example:
- Benign bone tumors and skeletal dysplasias.
- Juvenile idiopathic arthritis, which can alter a child’s blood flow.
- Cerebral palsy, which can cause nerve dysfunction.
- Fractures in the femur which heal in perfect anatomic alignment may result in overgrowth of the bone. This is thought to be due to the growth factors that facilitate fracture repair.
Less often, acquired leg length differences can also be idiopathic (having no known cause).
Unpredictable growth
In cases where a leg length difference is acquired during childhood, the difference in the leg lengths may be stable (stay the same) or may change as the child grows older. Unlike their congenital counterpart, acquired leg length differences are not usually predictable or proportional. The leg length difference could stay the same, get slowly worse, or rapidly worse.
What are the health concerns in a child with a limb length discrepancy?
The immediate concern is to measure the discrepancy and identify the cause to determine whether the child may have an underlying condition requiring treatment. These may include a growth plate injury, infection, a condition known as hemi-hypertrophy (where half of a person’s entire body grows larger than the other), or syndromes that involve irregular growth in other parts of the body.
When a leg length discrepancy is greater than 2.5cm, this causes increased energy expenditure to maintain a proper center of gravity when walking. This may cause pain in the hips, knees, ankles, or spine, and potentially lead to a visible limp and ultimately arthritis.
Leg length discrepancies that are less than 2cm typically cause no symptoms. In other words, the child doesn’t feel or look uneven, has no limp, and is not expected to develop hip pain, knee pain, ankle pain, back pain, arthritis, or any other problem.
What should parents do if their child has a limb discrepancy?
Leg length discrepancies of any kind rarely resolve on their own. If a leg length discrepancy is suspected, discuss this with your pediatrician. They will direct you to a pediatric orthopedic surgeon who can diagnose the condition and develop a treatment plan. (Find a surgeon at HSS who performs limb lengthening surgery.)
How is a limb length discrepancy in a child diagnosed?
Leg length discrepancies may be difficult to diagnose solely with a physical exam. A child’s orthopedic surgeon will order radiological imaging called EOS imaging. This imaging allows accurate measurements of leg length discrepancies and any other associated limb deformities that may need to be treated as well. (Read related content on leg deformity reconstruction surgery in children.)
How is a child with limb length discrepancy treated?
Treatment may be nonsurgical or surgical. The decision on precise treatment depends on the child’s age, the size and cause of the limb difference, and severity of symptoms – for example, gait (walking) problems or disruption of everyday activities. This includes predicted increases in a child’s limb discrepancies over time. The use of growth charts as well as an X-ray of the left hand make such predictions more precise.
Individualized treatment plans
At Hospital for Special Surgery, recommendations are made according to the following guidelines:
- When the discrepancy between the limbs is less than two centimeters (2cm) use of a shoe lift is appropriate.
- For those patients in whom the discrepancy ranges from 2cm to 5cm, a surgery called epiphysiodesis may be appropriate. This procedure slows the growth of the opposite leg or arm by altering the activity of the growth plate, thereby allowing the affected limb to “catch up” by the end of growth.
- For discrepancies greater than 3cm, however, limb lengthening may be an effective treatment choice.
In addition to these factors, the patient and family’s preferences and ability to follow up for the requisite postoperative care can play a role in treatment selection.
Determining a treatment plan for each individual child with a limb length discrepancy is based not only on the extent of the disparity at the time of diagnosis, but also on predicted increases in discrepancies over time. To make this prediction, the orthopedic surgeon considers the growth plate location, the age of the patient, the skeletal age of the patient (via radiograph of the left hand and wrist) and, in the case of a trauma or infection, the extent of injury to the growth plate.
In patients who have congenital limb anomalies of the leg, the predicted increase in limb length discrepancy can be calculated by comparing the short unaffected leg with the long unaffected leg. The percentage of growth arrest tends to remain constant during childhood. Use of CDC growth charts along with skeletal age facilitate prediction.
Shoe lifts
When a leg length difference is less than 2 cm and will remain so throughout the child’s growth, there are usually no symptoms and no visible limp. Treatment of any kind is often not required.
If the difference is small but the child feels uneven, or if they or their family observes a limp, a shoe lift inside or outside the shoe could be considered. It is possible to fit an internal lift, up to 0.5 cm to 1 cm, inside most shoes. For a larger leg length difference, the sole of the shoe can be elevated up externally. We usually recommend a full-length lift (across the whole shoe) for such differences, because using a wedge-shaped lift on the heel only can lead to shortening and tightness of the Achilles tendon.
While the shoe is worn, the legs will look and feel more equal. For large differences, a lift can even improve how the child walks/runs. It may, theoretically decrease the risk of complications from large leg length discrepancies that can develop in the long run.
Epiphysiodesis surgery to even out limb growth rates
If the length difference is already or is predicted to grow to between 2 cm and 5 cm, it is common to stop further the growth of the longer leg with a surgery called epiphysiodesis. This procedure causes arrest of the growth plate of the longer leg so the shorter leg can “catch up” over time. When children have this procedure, they can usually walk out of the hospital the same day with crutches for comfort. Many children are back to playing sports within a few weeks. The correction occurs over the course of a year or more. This surgery is typically performed in the last few years of growth, typically between the ages of 10 to 14.
Pediatric limb lengthening surgery
Various types of limb lengthening procedures are available for different conditions, ages, and length differences. A surgical treatment plan incorporates the current limb length difference as well as the difference that may occur in the future, since many leg length differences worsen over time.
When the difference is predicted to be above 5 cm, we commonly lengthen the shorter leg, either with an external metal frame or an internal metal nail. Sometimes more than one lengthening is required in childhood, as bones can only be lengthened about 5cm at a time with current technologies. Sometimes we combine techniques, with a lengthening of the shorter leg and epiphysiodesis to slow growth in the longer leg. Modern improvements in limb lengthening technology, specifically internal metal nails that lengthen the bone, have expanded our ability to take care of patients with larger leg length differences.
Ilizarov and intramedullary limb lengthening surgery in children
When limb lengthening surgery is indicated, orthopedic surgeons can safely and gradually lengthen the affected bone using what is known as the Ilizarov procedure (so named after its inventor, surgeon Gavriil Abramovich Ilizarov).
The Ilizarov procedure features a two-part process: osteotomy and distraction osteogenesis. First, the surgeon places an external fixator which is secured to pins and wires placed through the bone. Next, an osteotomy (cut) of the metaphysis is performed. This section of the bone experiences the fastest formation of new bone tissue during growth. The stage is set for the next part of the process, called distraction osteogenesis. Alternatively, osteotomy and distraction osteogenesis may be performed with an internal nail that is placed in the intramedullary canal. During either surgery, great care is taken to protect both soft tissue and the blood supply to the bone.


X-ray images of pediatric limb length discrepancy before and after surgery
Distraction osteogenesis is the process of very gradual separation of the bone at the site of the osteotomy incision and the formation of new bone tissue. Beginning five days after surgery, the physician − and then later the parents and/or child − adjust the external fixator or use a magnet to lengthen the intramedullary rod according to a precise schedule, usually three or four times per day. As the bone is “distracted” (pulled apart), new bone forms at the gap as part of the healing process. The rate of distraction is slow, with a standard increase of 1mm per day.
Fixation types
In pediatric patients, the orthopedic surgeon may use either a circular fixator based on the original Ilizarov frame or a telescoping intramedullary rod. Both devices allow simultaneous correction of the limb length discrepancy.
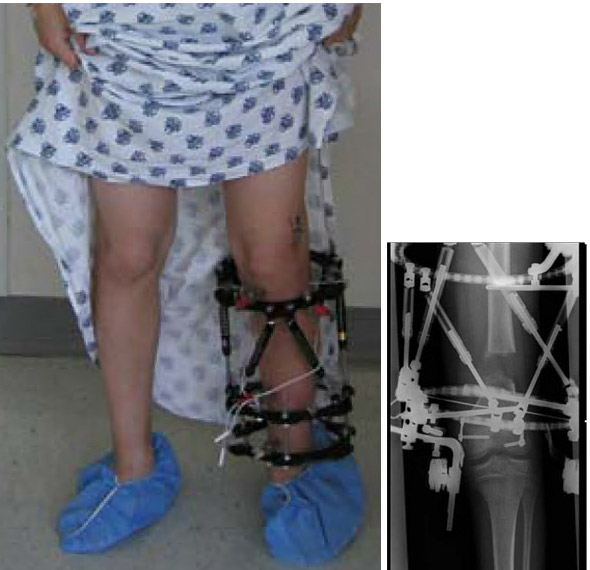
A child wearing a circular frame around the tibia (Taylor spatial tibial frame) and an X-ray of circular fixation frame around a femur, showing its internal workings.
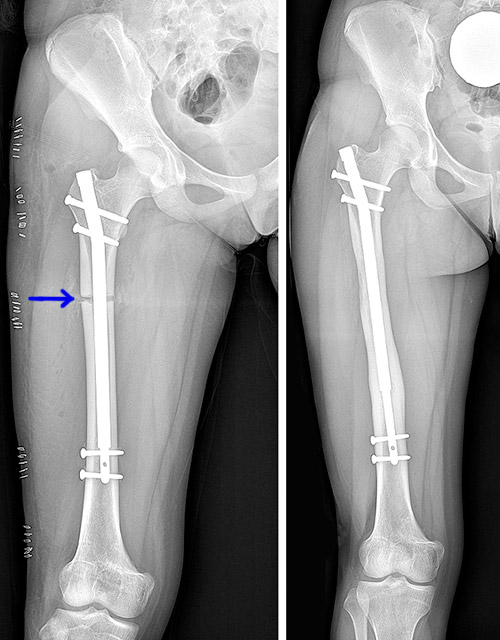
X-rays showing an implanted intramedullary rod for limb lengthening. The left image shows the osteotomy stage (at the blue arrow) while the image at right was taken after the lengthening and bone consolidation period.
Pediatric limb lengthening recovery and rehabilitation
Physical therapy plays a crucial part in the entire limb lengthening process. Patients meet with physical therapists before undergoing surgery and during their post-operative hospital stay − usually a period of 3 to 5 days. HSS physical therapists design the postoperative rehabilitation program and continue to oversee therapy throughout treatment. (Even those patients who live far away from the hospital benefit from this process, as HSS therapists work with local physical therapists or by virtual visits.)
Most patients see their physical therapists 3 times a week and are required to do home exercises for a minimum of 4 times a day. Physical therapy helps ensure that the surrounding soft tissues remain flexible as the patient’s bone length increases and that muscle strength is maintained.
Depending on the planned lengthening, treatment typically continues for between 30 and 60 days. Following this stage of treatment, the frame remains on the limb for an additional period of consolidation. This allows the regenerative bone to mature until it is capable of full, independent weight-bearing. When the surgeon has determined that this process is complete, the patient returns for removal of the frame, a day surgery that is usually performed with the patient under general anesthesia.
Complex limb lengthening may require multiple procedures over time
Depending on existing and predicted discrepancy, limb lengthening procedures may be repeated up to two or three-times during childhood. While the preferred lengthening for a given procedure is 5 or 6cm − amounts associated with the lowest number of complications − there is no specific limitation on additional surgeries, except for what’s appropriate and reasonable for patients and their families.
How safe for children is limb lengthening surgery?
In the hands of experienced orthopedic surgeons with limb lengthening expertise, this type of surgery has become highly predictable with an excellent safety profile. The most common complications are those involving soft tissue, where tightening or contractures can occur if soft tissue growth doesn’t keep up with bone lengthening. However, an appropriate physical therapy program should prevent or minimize this problem.
Irritation or superficial infection may also occur around the pin sites, but this is usually minor and easily treated with oral antibiotics. Moreover, owing to the gradual nature of the process, pain is usually minimal.
At HSS, this surgery is complemented by a staff of dedicated pediatric anesthesiologists and pediatricians. The physical therapy team has specialized training in the care of such patients. As with any orthopedic procedure, if you are considering limb lengthening, you want to choose an institution with a high volume of these surgeries. (Find a surgeon at HSS who performs limb lengthening surgery.)
How old must a child be to have limb lengthening surgery?
A common age to start a bone lengthening is around 8 years of age, but some children start as young as 4. The magnitude of lengthening in a young child is less than in an older child. Younger children cannot be lengthened with an internal nail, and typically require lengthening with an external fixator frame.
ReferencesReferences
- Dodwell ER, Garner MR, Bixby E, Luderowski EM, Green DW, Blanco JS, Widmann RF. Percutaneous Epiphysiodesis Using Transphyseal Screws: a Case Series Demonstrating High Efficacy. HSS J. 2017 Oct;13(3):255-262. doi: 10.1007/s11420-017-9549-5. Epub 2017 Apr 3. PMID: 28983218; PMCID: PMC5617815.
- Friend L, Widmann RF. Advances in management of limb length discrepancy and lower limb deformity. Curr Opin Pediatr. 2008 Feb;20(1):46-51. doi: 10.1097/MOP.0b013e3282f35eeb. PMID: 18197038.
- Goodbody C, Kedem P, Thompson M, Do HT, Mintz DN, Widmann RF, Dodwell ER. Reliability and Reproducibility of Subject Positioning with EOS Low-Dose Biplanar X-ray. HSS J. 2017 Oct;13(3):263-266. doi: 10.1007/s11420-017-9548-6. Epub 2017 Mar 1. PMID: 28983219; PMCID: PMC5617814.
- Garner MR, Dow M, Bixby E, Mintz DN, Widmann RF, Dodwell ER. Evaluating Length: The Use of Low-dose Biplanar Radiography (EOS) and Tantalum Bead Implantation. J Pediatr Orthop. 2016 Jan;36(1):e6-9. doi: 10.1097/BPO.0000000000000425. PMID: 25955169.
- McLawhorn AS, Sherman SL, Blyakher A, Widmann RF. Humeral lengthening and deformity correction with the multiaxial correction system. J Pediatr Orthop B. 2011 Mar;20(2):111-6. doi: 10.1097/BPB.0b013e328341bc87. PMID: 21099438.



